What is a horseshoe kidney?
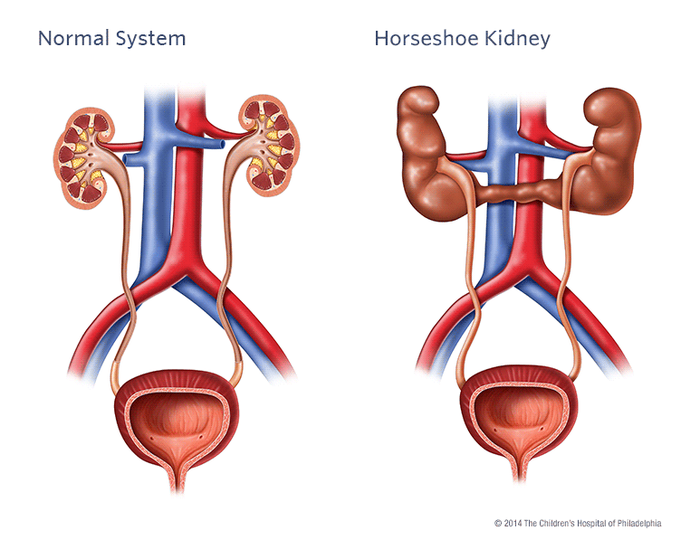
Normally, we have two separate kidneys which each have a single tube (called a ureter) that connects to the bladder. This tube drains urine from the kidney into the bladder from where you pass urine.
In some pregnancies, the kidneys do not develop normally. One such variation is known as a horseshoe kidney.
A horseshoe kidney means that, instead of having two separate kidneys on each side of the body the two kidneys are joined by their lower parts forming a U-shaped or horseshoe kidney.
You may be told that your baby has a horseshoe kidney during your pregnancy ultrasound scan or after your baby’s birth. You may need to go back to the hospital for further tests during the pregnancy and after birth.
You may instead be told your child has a horseshoe kidney if they he/she has had investigations due to urinary tract infections or abdominal pain.
The kidneys are part of the urinary system, which gets rid of things that the body no longer needs so that we can grow and stay healthy.
Horseshoe kidney is one type of congenital renal anomaly:
· congenital – the problem is present at birth
· renal – to do with the kidneys
· anomaly– different from normal.
Horseshoe kidney occurs due to an abnormality in the way the baby’s kidneys are developing while growing in the uterus (womb). It occurs between week 7 and 9 of the pregnancy. The cause of this abnormal development is not known. It is thought it may be due to a problem with faulty genes but no proven genetic cause has yet been found.
Children with chromosomal (genetic) disorders can be more likely to have horseshoe kidneys. These include children with syndromes such as Edward’s syndrome, Turner’s syndrome and Down’s syndrome.
Some children with horseshoe kidneys will have another anomaly (difference) in another part of their body. This can include: the spine, heart, intestines (gut) or skeleton (bone).
If it is known that your child has a chromosomal (genetic) disorder or there are concerns that your child has an anomaly (difference) in another part of his / her body then he / she may be referred to a geneticist. A geneticist is a doctor who specialises in genetic disorders. If your child has a horseshoe kidney this does not necessarily mean that he / she has a chromosomal disorder. If you have any concerns about your child, discuss this with your doctor.
How does horseshoe kidney happen?
While a baby is growing in the uterus (womb), the two separate kidneys normally move from the pelvis (hip area) to the flank area (just below the ribs at the back).
In horseshoe kidney, there is a variation in how this process happens. As the kidneys of the developing baby (the foetus) rise from the pelvis to the flank they join together (fuse). They fuse at the lower end of the kidneys. Instead of having two bean shaped organs there appears to be one U-shaped organ. In reality this is two separate kidneys that have a join between them, which still function as if they were two separate kidneys.
Horseshoe kidneys are normally lower down in the abdomen than normal kidneys.
Does horseshoe kidney affect how the kidneys work?
Horseshoe kidneys by themselves do not usually affect how the kidneys work. They may be an incidental finding on a scan (in other words, found out by accident). It is thought that this is the case in about a third of people with horseshoe kidneys and these people will have no signs or symptoms (see symptoms below).
How common is horseshoe kidney?
Horseshoe kidney occurs in about 1 in 500 children. They are more common in boys than girls.
Many people will have no signs or symptoms. However, due to the different anatomy (structure) of horseshoe kidneys they can predispose (make it more likely) for people to have other urinary tract problems, due to associated obstruction (blockage) and reduced urinary drainage. Your child may then have symptoms related to these problems. Other problems could include:
Pelvi-ureteric junction dysfunction or obstruction
A blockage of the urine flow at the area (junction) between the ureter and the pelvis of the kidney. Symptoms can include abdominal or back pain, a mass (swelling) in the abdomen, poor growth, bloody or cloudy urine
Vesicoureteral reflux
Urine travels back up the tubes from the bladder to the kidneys (it goes in the opposite direction it should do normally). This may be associated with symptoms of a urinary infection, bloody or cloudy urine.
Urinary tract infections
Symptoms can include fever, vomiting, pain on passing urine, abdominal or back pain, needing to pass urine more frequently.
Kidney stones
Also known as nephrolithiasis, these are collections of crystals that join together in the urinary tract. This can cause abdominal or back pain, pain that is sharp in nature, nausea or vomiting, fevers, bloody or cloudy urine.
Tumours
There are some reports to suggest that children and adults with horseshoe kidneys may be at slightly increased risk of some renal tumours or cancers, compared with those without horseshoe kidneys.
Diagnosis and tests in pregnancy
Horseshoe kidney can be found on a routine pregnancy ultrasound scan. The 20-week pregnancy ultrasound scan will look at the baby growing in the womb. If horseshoe kidney or other associated findings are found on this scan then further antenatal (before the baby is born) ultrasound scans may be required during the pregnancy.
Diagnosis and tests after birth
If horseshoe kidney is found on routine pregnancy or additional antenatal ultrasound scan, further scans may be needed after birth:
Ultrasound
After your baby is born, he / she will normally have an ultrasound scan, similar to the ones done during your pregnancy. How soon the ultrasound scan will be required after he/she is born will depend on what the antenatal ultrasound scan shows. The timing of this will be discussed with you.
DMSA scan (Dimercaptosuccinic Acid)
This is a type of radionucleotide scan. This means that a substance that gives out a type of radiation called gamma rays is injected into the blood stream. This substance is taken up by the kidneys and a special camera takes some pictures. This allows us to see how well the kidneys are functioning.
MAG3 scan (mercaptoacetyltriglycine)
This is another type of radionucleotide scan. In this scan a substance called mercaptoacetyltriglycine is injected into the blood stream. It is also linked to a substance that gives out a type of radiation called gamma rays. It is taken up by the kidneys and then a special camera takes pictures. This type of scan gives us information on how well the kidneys are functioning, but also on how well urine is draining from the kidneys down into the bladder.
MCUG (micturating cysourethrogram)
This is usually for babies and children who are suspected of having vesicoureteric reflux (urine travelling back up the tubes from the bladder to the kidneys). A special X-ray machine takes a series of images of the bladder while your baby is passing urine.
Urine tests
You, or a nurse, would need to collect some of your child’s urine in a small, clean container for a urine test. A dipstick will be dipped into the urine – this is a strip with chemical pads that change colour depending on what substances are in the urine. The sample may also be sent to a laboratory for more accurate tests.
Blood tests
As well as various scans, your child may have some blood tests. This gives an idea of how well the kidneys are working.
Horseshoe kidney treatment
If your child has no symptoms or associated problems then treatment may not be needed. It is, however, important to monitor your child for symptoms of the associated problems as outlined above (abdominal or back pain, abdominal mass, fever, vomiting, poor feeding, pain on passing urine, bloody or cloudy urine). If these occur, seek medical advice.
There is no cure for horseshoe kidney. If your child has a horseshoe kidney and he / she is having symptoms then he / she can have “supportive treatment”. Supportive treatment is treating the symptoms of a problem, such as pain, but not being able to cure or fix the issue that is causing it.
Surgery
Occasionally, surgical procedures are required due to complications such as kidney stones, pelvi-ureteric junction dysfunction or obstruction or vesicoureteral reflux. If your child has some of these associated problems you may be referred to a urologist for a review. A urologist is a surgeon who specialises in the urinary tract.
Surgical interventions would be discussed with you by your urologist if they were required.
Kidney stones
Sometimes tiny stones pass out on their own just by going for a wee. Smaller stones can sometimes travel down the ureter and get blocked. Stones that won't pass on their own can be broken up with lasers. Fragments may then be retrieved with baskets. Most of the time surgeons are able to do these operations using cameras that go through your child's urethra. Sometimes the only way to get them is by putting a tube straight into the pelvis of the kidney and getting the stones out that way. Often after operating for stones, surgeons would leave a tube called a stent in, that goes from the kidney to the bladder to make sure that the ureter doesn't get blocked.
Pelvi-ureteric junction dysfunction or obstruction
Most of the time pelvi-ureteric junction dysfunction or obstruction does not need an operation, if the kidney is able to drain well. Sometimes the junction is so tight that an operation is needed to cut out the tight junction and join the kidney back on to the ureter tube. This then lets the kidney drain well.
Vesicoureteral reflux
This does not usually require surgical treatment. When vesicoureteral reflux is associated with frequent urinary tract infections that do not respond to preventer antibiotics, an endoscopic (key hole) anti-reflux procedure may be advised, where a gel is injected into the area where the ureter enters the bladder to help prevent urinary tract infections.
Monitoring and follow up
Your child should be able to do all of the things that other children their age do. Your child should be able to go to nursery and school, play with other children and stay active.
Your child may be followed up by healthcare professionals, usually at a hospital. This may be a paediatrician (a children’s doctor), a paediatric nephrologist (a specialist in kidney care) or a paediatric urologist.
Further support
This can be a difficult and stressful experience for you and your family. If you have any concerns or need additional support, speak with your doctor or nurse.