Some boys are born with posterior urethral valves (PUV). These are extra flaps of tissue that are in the tube that carries urine out of the body. Babies with PUV may not be able to wee normally – both while growing in the womb and after they are born.
PUV may be suspected during pregnancy, on the antenatal ultrasound scan. PUV is diagnosed after birth with some tests. In some cases, they are diagnosed when a boy is older.
PUV need to be removed by surgery. Sometimes, other treatment is needed. Boys who have had PUV may have problems in their kidneys and/or bladder later in childhood, and will need follow-up throughout their lives.
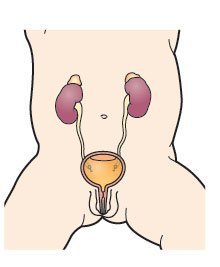
About the urinary system
The urinary system gets rid of things that the body no longer needs so that we can grow and stay healthy.
The kidneys are bean-shaped organs. They filter blood and remove extra water and waste in urine (wee). Most of us have two kidneys. They are on either side of our spine (backbone), near the bottom edge of our ribs at the back.
The two ureters are long tubes that carry urine from the kidneys to the bladder.
The bladder is a bag that stores urine until we are ready to pass urine (have a wee). It sits low down in the pelvis.
The urethra is a tube that carries urine from the bladder to the outside of the body.
Symptoms and complications
PUV can cause serious problems because they stop – or partially stop – urine flowing out of the bladder and through the urethra. After the PUV are removed by surgery, some boys have no symptoms or complications. In other cases, they can cause other problems shortly after birth or later in life, which need further treatment.
- Occasionally, newborn babies are unable to breathe properly because the PUV leads to problems with their lungs. They need special care after birth to help them breathe.
- PUV may cause bladder problems, and some boys have problems passing urine. A few will need to use a catheter (a long, thin tube that is placed through the urethra) to help empty their bladder.
- PUV may cause the kidneys to swell – this is called antenatal hydronephrosis, and is a common problem for babies in the womb. Occasionally, this causes more serious problems.
- Boys with PUV may be more likely to get urinary tract infections (UTIs) when germs get into the urine and cause infection and illness. These are treated with medicines. In some cases, boys with PUV get a serious infection in their kidneys or in their blood.
- PUV may cause vesicoureteral reflux (VUR) – when urine refluxes (goes back up) the wrong way towards or into the kidneys
- Occasionally, PUV can cause, or happen with, more serious problems with the kidneys.
More about symptoms and complications
Causes
PUV are extra flaps of tissue that are in the back (posterior) part of the urethra. They develop while a baby boy is growing in the womb.
PUV are the most common type of bladder outlet obstruction in newborn babies. This means that they stop (obstruct) the flow of urine out of the bladder.
PUV are rare. In the United Kingdom, it is estimated that one newborn boy in 5,000 to 8,000 has PUV. It is not known why some boys have PUV. They are not inherited from the mother or father, or caused by anything that the mother does during her pregnancy.
PUV may happen with other anomalies or abnormalities in the urinary system. This may mean that one or both kidneys or ureters do not develop properly.
Read more about the urethra in boys and PUV
PUV may happen with other anomalies or abnormalities in the urinary system. This may mean that one or both kidneys or ureters do not develop properly.
Will it affect other family members?
Doctors do not think that PUV runs in families. If one of your children has PUV, it is unlikely that another of your children or another family member will get them.
Test and diagnosis
PUV may be suspected or diagnosed (identified) at different times in a boy’s life.
Before birth
The 20 week antenatal ultrasound scan looks at your baby growing in the womb. It also measures the amount of amniotic fluid (or liquor), the liquid that surrounds your baby, which is partly made up of his urine. PUV cannot be seen in the scan. They may be suspected in a boy if there are signs of a bladder outlet obstruction – that urine is not flowing out of the bladder.
You may need to go back to the hospital for more ultrasound scans during pregnancy. You may be referred to specialist healthcare professionals, such as a paediatric urologist (a surgeon who treats children with problems of the urinary system) or a paediatric nephrologist (a doctor who treats children with kidney problems).
After birth
If the antenatal scan(s) showed signs of a blockage affecting the flow of urine, your child will need tests to find out whether he has PUV or another condition. Some babies show signs, such as dribbling urine or having a larger bladder that feels like a lump in the tummy.
Later in life
In some boys, PUV are not diagnosed until later in life. Signs of PUV include problems passing urine, wetting themselves or urinary tract infections. Your child will need some tests to find out whether he has PUV.
More about tests and diagnosis
Treatment
Before birth
In most cases, there is no treatment before birth. In a small number of cases, an operation may be recommended during pregnancy. This aims to drain urine out of the baby’s bladder and into the amniotic fluid (or liquor) that surrounds the baby.
Where is my baby or child treated?
Some babies need to go into a neonatal unit, an area of the hospital for newborn babies who need support, for tests and treatment. Older children are treated in a paediatric unit, a special part of your hospital, for children. Some children need to be transferred to another hospital where specialist services are available.
After birth
The first treatment is to drain urine from the bladder. This helps reduce the risk of long-term problems with the bladder and kidneys. A catheter (a long, thin tube) is placed through the urethra (from the tip of your child’s penis), or sometimes through the wall of the tummy, into the bladder, and urine flows out.
All boys need an operation to remove the PUV – this is called a PUV resection. This will happen shortly after diagnosis.
About the future
Follow-up
All boys who have been treated for PUV will need follow-up throughout their lives, to check for any long-term problems with their kidneys or bladder.
Long-term effects
Some boys will have no long-term problems. Some will need further care, such as using special equipment to pass urine and make sure their bladder is emptied.
Some boys with PUV may progress to later stages of chronic kidney disease (CKD) – their kidneys gradually stop working as well as they should; this usually happens slowly over many years. Some children with CKD may progress to final stages of CKD (kidney failure), and need specialist treatment.
If your child has CKD, you and your child will learn more over time about how to help manage the condition and what to expect.